- DKA is a dangerous complication of T1 diabetes occurring due to an absence of insulin causing significant ketogenesis
Definition
-
- DKA is sefined as a triad of:
- Hyperglycaemia (>11mmol)
- Metabolic acidosis (pH < 7.3, HCO3 <15mmol)
- Ketosis – capillary ketones (>3mmol/L)
- DKA is sefined as a triad of:
- All 3 must be present for it to be DKA
- NB May present with euglycaemic DKA
- This is often DKA which has been partially self-treated by the patient who has recognised it coming on
- Also rarely found in patients on SGLT2 inhibitors as the glucose is peed away (uncommon as SGLT2 inhibitors are rarely used in T1DM)
- NB May present with euglycaemic DKA
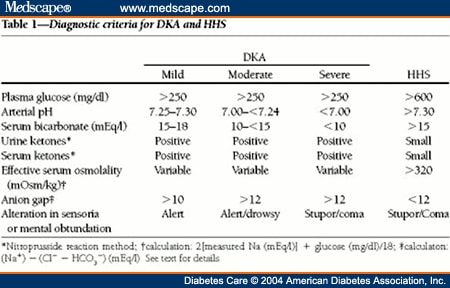
- DKA is divided into 3 grades of severity mainly based on the degree of ketosis + acidosis
Epidemiology
- DKA is the most common endocrine emergency
- Mortality rate of 10%
- Usually affects T1DM
- Can also occur in longstanding T2DM where virtually no insulin is being made
Pathogenesis
(see metabolic changes in T1DM to contextualise this)
- Absence of insulin independently causes two things:
- Hyperglycaemia due to a lack of glucose uptake and gluconeogenesis
- Gluconeogenesis which is normally inhibited by insulin
- Lipolysis/proteolysis occurs instead of glycogenolysis when there is no insulin
- The ketogenic products are metabolised in the liver to form acidic ketones
- There are many ketones – the main relevant one is 3-hydroxybutrate which is detected
- Results in ketoacidosis
Aetiology
DKA can present in several scenarios
- DKA is often the first presentation of T1DM
- Often follows the interruption of insulin therapy in T1 patients when not eating
- Hence, ‘sick day rules’ are crucial in prevention
- Other causes
- Acute illnesses (infections and Infarcts)
- Stress
- These often combine with insulin interruption)
- The trigger is idiopathic in around 40% of cases
Clinical PresentatioN
- Ketogenesis (Ketones Waste the Gut, Brain, and Heart) – note that these features aren’t found in HHS
- Lipolysis/proteolysis causes weight loss and muscle wasting
- GIT:
- N&V
- Abdominal pain
- CNS:
- Generally weakness, fatigue
- Drowsiness, Confusion
- Blurred vision
- Coma
- CVS:
- Hypotension
- Ketotic breath (pear drops)
- Acidosis
- Kussmaul respiration to compensate for metabolic acidosis may be seen
- A type of deep ‘sighing’ hyperventilation
- Kussmaul respiration to compensate for metabolic acidosis may be seen
- Hyperglycaemia – Sx of this will not always occur
- Profound dehydration and electrolyte loss due to massive osmotic diuresis (as DKA coincides with severe hyperglycaemia)
- Features of dehydration – see separate
- CNS features (similar to those above)
- Profound dehydration and electrolyte loss due to massive osmotic diuresis (as DKA coincides with severe hyperglycaemia)
Complications of DKA
- The symptoms above result in a variety of potentially fatal complications
- These occur either iatrogenically or due to micro and macro vascular obstruction leading to ischaemia
- Remember (TAHOPS) – 2 of these are iatrogenic
- Thromboembolism – due to increased viscosity of blood can be either arterial or venous
- ARDS
- Hyper/hypokalaemia
- Hypokalemia if too much insulin is given and hyperkalemia if not enough
- Cerebral Oedema can occur if osmolality is brought down too quickly (e.g. by giving too much fluid too quickly)
- Main cause of death in these patients
- Therefore lower glucose slowly (3mM/hour)
- Aspiration Pneumonia with depressed consciousness + vomiting
- Shock with depressed consciousness + vomiting
Assessment
History and examination
- History:
- Any precipitating factor?
- Previous management if a known diabetic?
- Physical examination:
- Look for causes and symptoms of DKA
- Respiratory exam – pneumonia?
- Cardiac exam – esp consider dehydration and MI
- Abdominal exam – acute abdomen
- Neurological exam + GCS
Investigations:
The following must be both investigated at diagnosis and monitored regularly after this
- Bedside
- Obs – Signs of dehydration
- ECG
- Insulin deficiency causes hyperkalemia – tall tented T waves, PR interval, P wave, etc
- Also excludes MI
- Urine dipstick
- Urine Ketones (at least ++) – NB this is delayed compared to capillary ketones
- Urine Glucose
- Urine output is also required for dehydration
- Blood
- Capillary tests are done first
- Blood capillary glucose
- Blood capillary ketones
- Serum tests
- Serum BGL – more reliable than capillary/blood gas readings
- Serum Ketones (>3.0)
- NB these clear faster than urinary ketones
- U&Es:
- K+
- Hyperkalemia due to loss of insulin and acidosis both allowing K+ to move out of cells.
- Total K+ may be low as excretion also increases with hyperglycaemia but will typically be high due to metabolic shift
- Monitor during treatment – see below
- Urea and creatinine raised – dehydration
- Na+ can be high or low
- Calculate anion gap if possible
- K+
- Clotting – informs thromboprophylaxis
- Septic screen – if suspecting infection (DKA does also cause a SIRS response
- FBC
- CRP/ESR
- ± blood cultures
- ?troponin – if suspecting MI
- ABG/VBG is crucial to show acidosis as well as electrolytes and glucose
- Capillary tests are done first
- Imaging
- CXR if suspecting infection
Management of DKA
- There are 3 steps to the management of DKA:
- Resuscitate
- I.e. treat and prevent complications (ABCDE)
- Reverse the DKA
- Treat hyperglycaemia (aim for <14mM at a rate of <3mmol/hr)
- Treat ketosis (aim for ketones <0.3mM
- Teeat acidosis (aim for VBG pH>7.3)
- Treat hyperkalaemia/hypokalaemia (aim for 3.5-5.5mmol)
- Secondary Prevention (Long-term treatment):
- Find and treat the precipitant and underlying conditions
- Resuscitate
- Monitoring is key to consider at all stages
- ITU referral is generally indicated by
- Severe derangement of DKA parameters (e.g. ketones, pH, potassium – but not glucose)
- Poor general health (BP, HR, GCS, SaO2)
Resuscitation
- Patients may present with life-threatening complications
- Would take an ABC approach
- As part of this, some of the DKA management would be initiated
- Mainly aim to prevent the complications – thrombosis, hypokalemia/hyperkalemia, ARDS, aspiration pneumonia
- An ABCDE approach may show the following:
- A
- Patient may be unconscious
- B
- Patient may be at risk of ARDS or aspiration pneumonia
- NGT can drain if vomiting or disturbed GCS to prevent aspiration pneumonia
- Patient may be at risk of ARDS or aspiration pneumonia
- C
- Fluid therapy (see DKA)
- Start with a STAT dose if shocked
- Prevent cerebral oedema
- (see above) bring down osmolality (glucose, sodium) slowly
- Hypokalaemia – need continuous ECG monitoring
- Fluid therapy (see DKA)
- D
- Glucose obviously is checked
- Consciousness may be disturbed and must be formally assessed (GCS)
- E
- Thromboprophylaxis may be done using heparin
- A
Reversing DKA
-
- 3 main interventions (RIP) are done at the same time followed by monitoring and complication prevention (MC)
- End-points for DKA reversal:
- BMs <11
- Aim to drop by ≤3mmol/hour – prevents cerebral oedema
- Once bgl <14mmol, add glucose (NB this ≠ a sliding scale as the insulin remains given at a constant rate)
- Ketones <0.5
- Aim to drop by >0.5mmol/l/hr
- PH neutral
- Aim to increase HCO3 by 3mmol/l/hr
- BMs <11
- Usually should be out of DKA by 12 hours – ketone free and E&D
- Rehydrate:
- Replace lost fluid to treat dehydration and lower glucose/Ketones/K+
- Usually lose about 6L has been lost
- 0.9% Saline is typically used
- Titrate to BP but usually give 6L – 1L every 1/2/2/4/6/8 hours
- If shocked, a STAT bolus of 500ml may be given before the 6L
- Add 10% glucose when [blood glucose] <14mmol/l to prevent hypoglycaemia (whilst still correcting the dehydration)
- Usually given at a rate of 125ml/h (i.e. a bag over 8 hours)
- Not always necessary
- HCO3 is only used if severely acidotic – pH <7.0
- Beware cerebral oedema which occurs when bringing down serum osmolality too fast (i.e. urea, K+, Na+, and glucose)
- Especially consider sodium which accounts for most of the serum osmolality
- Replace lost fluid to treat dehydration and lower glucose/Ketones/K+
- Insulin (Fixed Rate Infusion) – This treats the DKA, hyperglycaemia, and suppresses lipolysis very well
- Dosage
- Actrapid 0.1units/kg/hr is used
- Given in 50u/49.5ml saline (i.e. 1u/ml)
- Nowadays some areas may give rapid-acting analogues instead
- Increase by 1 unit/hr if ketones + glucose are not improving
- Transfer to SC insulin once DKA is resolved and patient is eating and drinking and aims have been met (see below)
- If patient is not ketotic but also not E&D, move to a sliding scale
- NB: previously prescribed basal insulin is continued
- However, discontinue the mealtime bolus insulin
- Continue the basal because it takes a while to reinstate it after it is stopped
- Actrapid 0.1units/kg/hr is used
- Dosage
- Potassium replacement
- Patient will (usually) be initially hyperkalemic in the blood but actually have low total potassium in the body.
- Redistribution with fluid replacement and insulin moves K+ out of the blood and can therefore rapidly cause iatrogenic hypokalemia
- Give potassium fluids with each bag of NaCl after the first bag
- Usually come as premixed bags
- Titrate according to blood [K+] measured by 2-hourly VBG
- Aim between 3.5-5.5 – hospital will give rates adjusted to the VBG
- 20mM per L of saline is usually given if normokalemic and no K+ is given if >5.5mmol
- Can give a max of 20mM/hour
- Ensure patient is on ECG monitoring
- Patient will (usually) be initially hyperkalemic in the blood but actually have low total potassium in the body.
- Regular Monitoring is necessary throughout the DKA treatment:
- Hourly BGLs – aim for a max drop of 3/hr
- Hourly Capillary ketones
- 2-Hourly VBG – measures K+ (titrate), Na+/glucose (cerebral oedema), pH
- Catheterisation – accurately indicates hydration level
- ECG for hyperkalemia
Further treatment (once DKA has resolved stable patient)
- The patient is regularly reassessed and weaned off insulin when appropriate
- Usually done by Diabetic Specialist Nurses
- Usually switch over to SC insulin once the patient is eating
- If basal-bolus regimen:
- Start on basal insulin (if not previously on it anyway) while still on the infusion
- Start mealtime insulins (short-acting) with the next meal – stop the IV insulin after the meal
- If on a premixed regimen, it is a bit more complicated
- May or may not be stopped during the DKA protocol
- Usually start with the next meal
- NB premixed is rare
- If basal-bolus regimen: